Postdoctoral Research Fellow - Health Services Research
Predicting CBT modality, treatment participation, and reliable improvements for individuals with anxiety and depression in a specialized mental health centre: a retrospective population-based cohort study




This project explores how people with anxiety and depression respond to different types of Cognitive Behaviour Therapy (CBT) — whether done one-on-one, in a group, or online. Using real-world data from Ontario Shores Centre for Mental Health Sciences, we analyzed which personal and clinical factors help predict who benefits most from each therapy format
and who is more likely to complete treatment. Our goal is to make mental health care more personalized, accessible, and effective by helping match the right kind of therapy to the right person at the right time.
In collaboration with Ontario Shores Centre for Mental Health Sciences and Ontario Tech University, funded by Green Shield Canada.


Abstract:
Cognitive Behaviour Therapy (CBT) is one of the most successful therapeutic approaches for treating anxiety and depression. Clinical trials show that for some clients, internet-based CBT (eCBT) is as effective as other CBT delivery modes. However, the fidelity of these effects may be weakened in real-world settings where clients and providers have the freedom to choose a CBT delivery mode and switch treatments at any time. The purpose of this study is to measure the CBT attendance rate and identify client-level characteristics associated with delivery mode selection and having reliable and clinically significant improvement (RCSI) of treatment in each delivery mode in a real-world CBT outpatient program.
Methods:
This is a retrospective cohort analysis of electronic medical records collected between May 1, 2019, and March 31, 2022, at Ontario Shores Centre for Mental Health Sciences. Regression models were used to investigate the impact of individual client characteristics on participation and achieving RCSI of different CBT delivery modes.
Results:
Our data show a high attendance rate for two and more CBT sessions across all modalities (98% of electronic, 94% of group, 100% of individual, and 99% of mixed CBT). Individuals were more likely to enter mixed and group CBT modality if they were younger, reported being employed, and reported higher depression severity at the baseline. Among the four modalities of CBT delivery, group CBT clients were least likely to have RCSI. Of those who started sessions, clients were significantly more likely to experience RCSI on the Patient Health Questionnaire (PHQ)-9 and the Generalized Anxiety Disorder (GAD)-7 if they were employed, reported more severe symptoms at baseline, and were living in the most deprived neighborhoods.
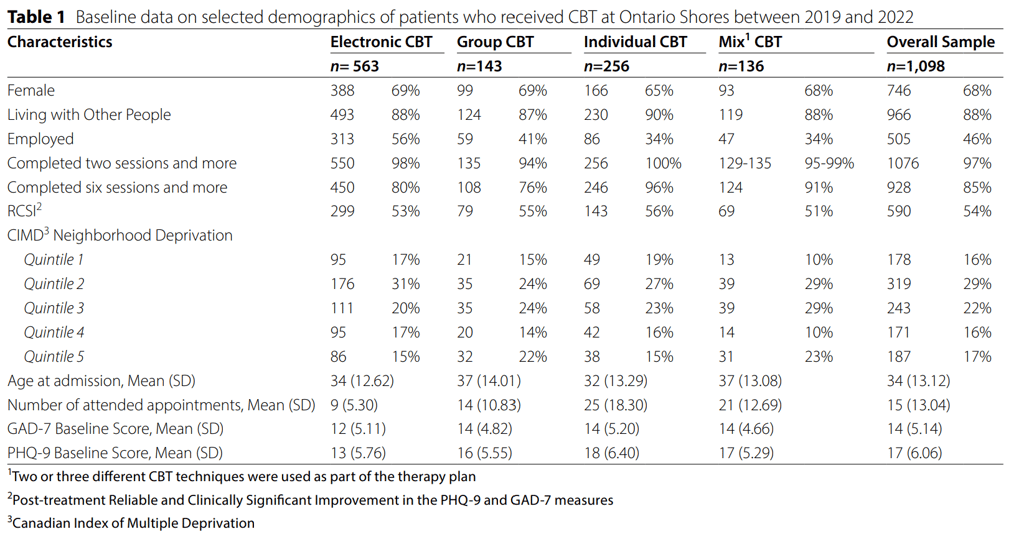
Table 1 shows descriptive statistics for clients receiving electronic (n=563), group (n=143), individual (n=256), and mixed CBT (n=136). The findings are based on the completed (n=711) imputed data (n=387) for all 1,098 clients receiving CBT at Ontario Shores between May 1, 2019, and March 31, 2022. The analysis of baseline PHQ-9 and GAD-7 scores reveals a consistent pattern across most Cognitive Behavioral Therapy (CBT) modalities. However, an exception is observed in the case of eCBT. In the eCBT group, the average baseline GAD-7 score was 12 (SD=5.1), compared to an average of 14 in the other groups (F-statistic=9.209, p=5.55e-06. This places the average score within the category of ‘Moderate anxiety’ (10–14 range) according to the GAD-7 scoring guidelines [14]. In the eCBT group, the average baseline PHQ-9 score was 13 (SD=5.8), compared to an average of 16 to 18 in the other groups (F-statistic=25.45, p=1.21e-15) This information suggests that individuals participating in or being assigned to eCBT may, on average, exhibit more moderate levels of depression compared to counterparts in other CBT modalities.
Among all modalities, clients undergoing individual CBT exhibited the highest attendance rate averaging 25 sessions. Clients on average were young females living with others in a moderate socioeconomically deprived neighborhood (Q2 and Q3). They were mostly unemployed, and they had moderate anxiety (10–14 GAD-7 scores risk level) and moderately severe depression (15– 19 PHQ-9 scores risk level) on average, with the eCBT cohort scoring the lowest symptom severity. At the end of treatment, more than half of the clients have attained RCSI (56% individual CBT, followed by 55% group, 53% electronic, and 51% mixed CBT).
Table 2 displays coefficient results of each CBT modality in comparison to our baseline modality which is eCBT. Employment was associated with lower probability of receiving individual CBT (OR=0.49, 95% CI [0.35–0.68]), mixed CBT (OR=0.5, 95% CI [0.33–0.75]), and group CBT (OR=0.64, 95% CI [0.44–0.95]). Older age was a predictor of entering into the mixed modality (OR=1.02, 95% CI [1.01–1.04]) and group CBT (OR=1.02, 95% CI [1.00-1.03]) versus eCBT. Although the results of CIMD neighborhood deprivation index were inconsistent, living in the fifth quantile (Q5), which identifies the most deprived neighborhood [20], was associated with participation in mixed CBT (OR=2.24, 95% CI [1.08–4.63]). Compared to eCBT, the severity of the client’s depressive symptoms at baseline was a positive predictor of receiving individual (OR=1.15, 95% CI [1.11–1.20]), mixed (OR=1.08, 95% CI [1.03–1.13]), and group CBT (OR=1.06, 95% CI [1.02–1.11]).
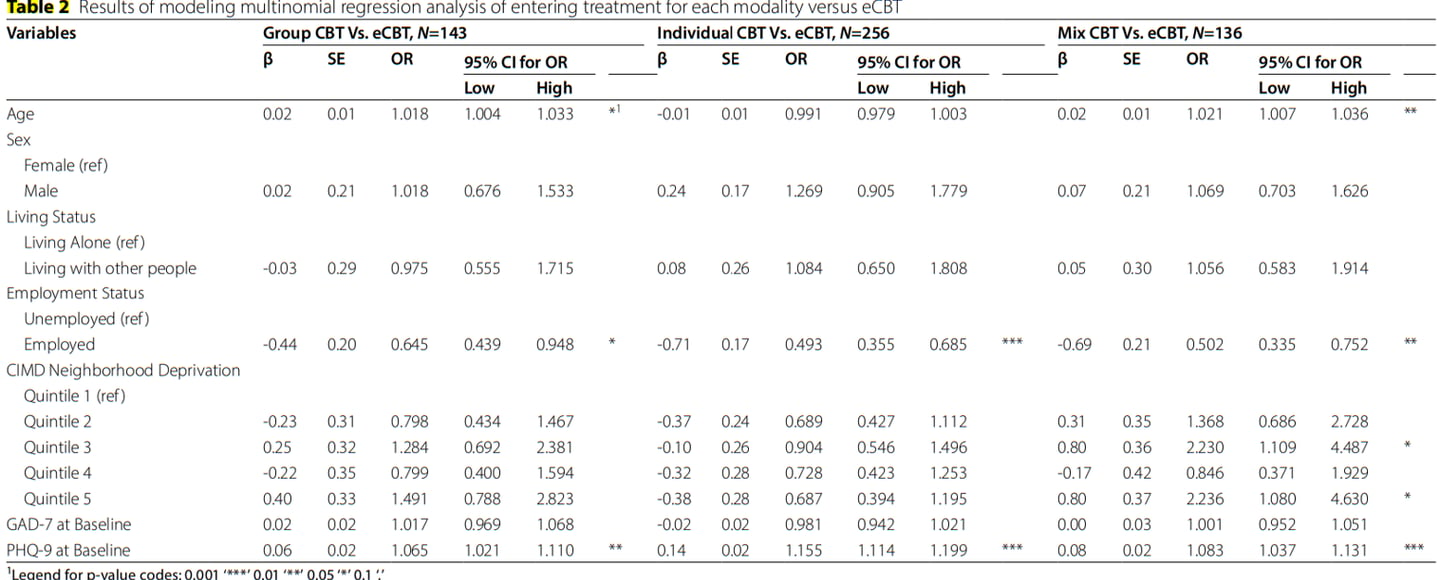
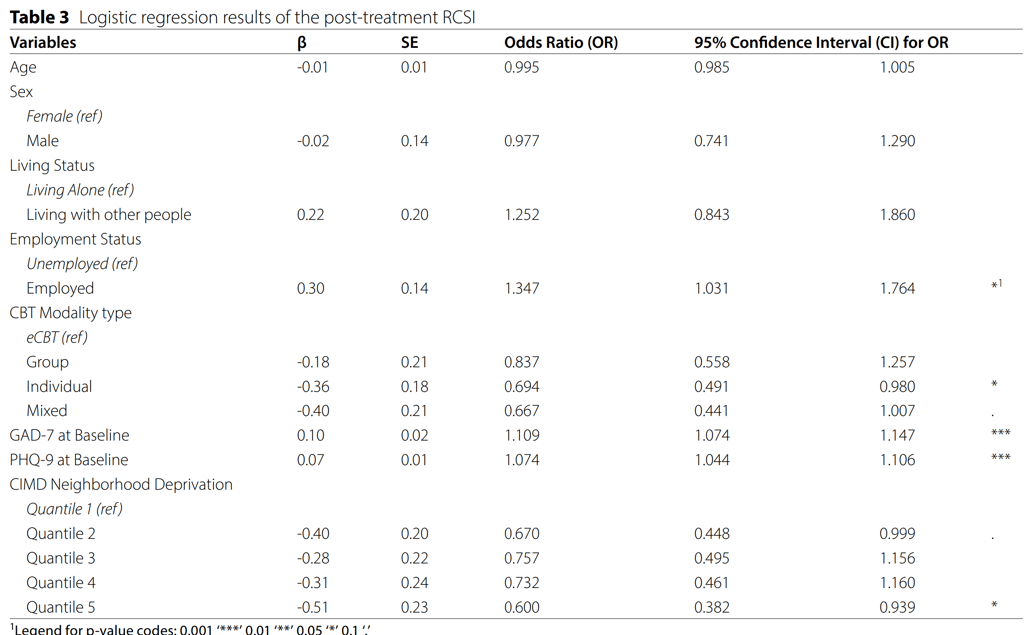
Table 3 shows the results of a logistic regression analysis on the post-treatment RCSI outcome. From our sets of demographic variables employment (OR=1.35, 95% CI [1.03–1.77]) was significant in predicting treatment success in terms of having RCSI. As expected, both baseline PHQ-9 (OR=1.11, 95% CI [1.07–1.15]) and GAD-7 (OR=1.07, 95% CI [1.04–1.11]) are significantly associated with RCSI. Regarding the modality type, participating in individual (OR=0.69, 95% CI [0.49–0.98]) and mixed CBT (OR=0.67, 95% CI [0.44–1.01]) modalities decreased the probabilities of having RCSI relative to eCBT. Despite the inconsistency of the CIMD quantile results, living in the most deprived neighborhood (Q5) (OR=0.60, 95% CI [0.38–0.94]) decreased the likelihood of having post-treatment RCSI.
Our team
1) Faculty of Health Sciences, The University of Ontario Institute of Technology, Oshawa, Ontario, Canada
2) Ontario Shores Centre for Mental Health Sciences, Whitby, Ontario, Canada


Afsaneh Roshanghalb (1,2)
Bojay Hansen (1)
Michael W Bes (1,2)
David Dudoler (1,2)
Get in touch
Phone
info@afsa.com
© 2025. All rights reserved.